
Nicholas Peat
24 December 2025
In my first article, I spoke about how my health crisis forced me to stop, listen, and reassess a life spent constantly pushing forward.
This second part of the journey goes deeper, deeper into the place where much of that damage had quietly been building for years: my gut.
For many men, gut health is simply about their digestion, with recognising possible minor symptoms of bloating, pain, or additional trips to the bathroom. But what I’ve learned, both personally and professionally, is that the gut sits at the centre of physical performance, emotional regulation, immunity, and resilience.
When the gut struggles, everything else follows.
Ignoring the Early Signals
Before my bowel perforation, I knew something needed to change.
There were internal nudges, moments of awareness where I recognised that my lifestyle, stress levels, and fuelling weren’t sustainable. But like many men, I ignored them. I was busy. I was working. I was providing for my young family. I pushed those thoughts aside.
Then the perforation happened, and that internal voice disappeared. The consequences were no longer hypothetical. This was the reality of not listening.
Fuelled, Busy… and Undernourished
At the time, my lifestyle looked productive but was physiologically depleted.
- A heavily processed vegetarian diet
- Very low omega-3 fatty acid intake
- Vitamin D deficiency from working indoors
- No supplementation
- High stress from A&E shifts, medical teaching, and renovating a flat alone
On paper, I was functioning. In reality, my gut, immune system, and nervous system were under constant strain.
Eventually, that strain became inflammation, and inflammation became an internal injury.
Radical Change
After surgery, I removed ultra-processed foods, sugar, bread, pulses, legumes, and most plant-based proteins almost overnight. My diet became extremely restricted, mainly just fruit and vegetables.
In the first 2-3 weeks, I found it very difficult to avoid sugar and to eat a wide range of foods. However, I soon adjusted to my new dietary pattern. It’s important to note that I was also resting, sleeping, and on sick leave for the first 3 months, which significantly contributed to my recovery.
3-4 months after surgery, I was offered immunosuppressive medication, commonly used in Crohn’s management, at the time. While these treatments are essential for many, I struggled with the idea of long-term reliance on prescription medication, frequent blood tests, and ongoing monitoring.
I initially accepted the prescription, but after having time to think about what I would be entering into long-term. I then made a conscientious decision not to take it, but wanted to gain support in my decision. I discussed my pathology report with a consultant pathologist colleague, who recommended I communicate my decision in writing with my consultant. We agreed I could trial a nutrition-led approach, with annual MRI and colonoscopy monitoring.
Thankfully, my results consistently showed no active Crohn’s disease.
When “Clean Eating” Isn’t Enough

For that first year, I had restricted myself to a diet of mainly just fruit and vegetables. I may have looked and felt incredibly healthy, and thought at the time I was doing the right thing, but I had not considered that I was actually under-fuelling. I lost significant weight and muscle mass.
At the time, I wasn’t trained in nutrition. I had no dietitian, psychologist, or fitness support. I was navigating this part of my recovery alone. I missed the foods I once ate and wanted to increase my protein intake, so I gradually expanded my food choices in a healthy manner.
Over time, I slowly reintroduced:
- Pulses and plant proteins
- Occasional bread, cheese and sugar
- Very infrequent ultra-processed foods
The difference was intention. The less healthy foods no longer dominated my diet as they had previously, and the foundation of my diet became whole foods, healthy fats, fibre diversity, and an overall balanced plate of nutritional food.
The Missing Piece: Mental and Emotional Load
What I hadn’t fully appreciated was how deeply my mental health was driving my gut health.
As a junior doctor with a young family, constant financial pressure, disrupted sleep, and chronic stress, my nervous system lived in survival mode.
Over time, I began addressing my mental and spiritual wellbeing, learning to shift focus away from constant worry. This wasn’t quick. Anxiety doesn’t resolve overnight. This took patience, time and true dedication.
Once my mind stabilised, I then struggled to reintroduce movement. I hadn’t exercised properly for years, but I knew how to. After several years, I started slowly and then progressively added more aerobic, strength training, and resistance training to my routine.
I went from 58 kg to 78 kg, gaining a healthy mix of muscle and fat mass. Today, I’m fitter and stronger than I was in my twenties.
The Gut–Brain Axis: A Two-Way System
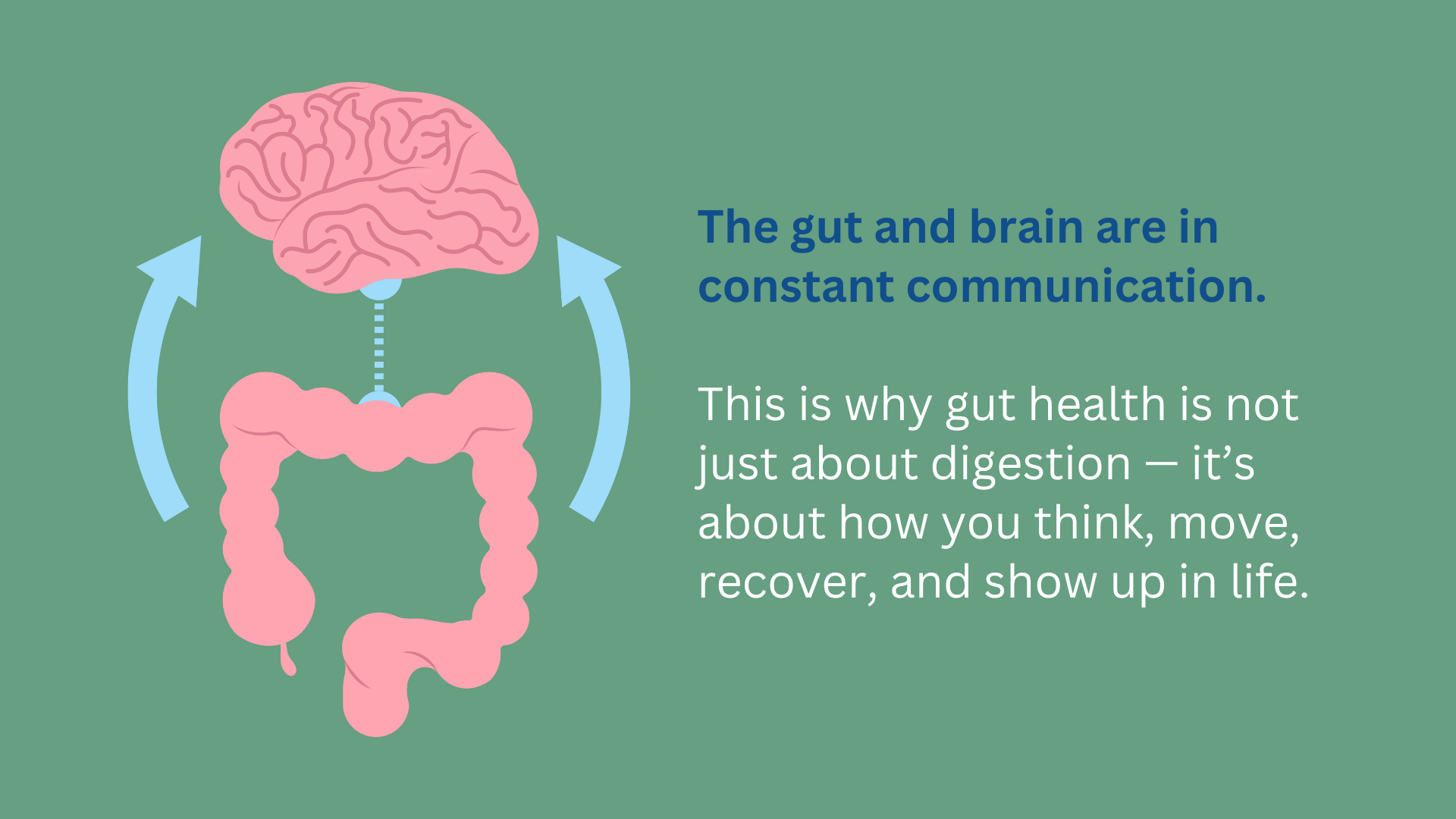
We now understand that the gut and brain are in constant communication via neural, hormonal, and immune pathways, known as the gut–brain axis. Even though there has been much medical research into the gut-brain axis, there is still so much more we need to understand and can expand on.
In my own case:
- Chronic stress raised cortisol
- Cortisol increased inflammation
- Inflammation disrupted gut integrity (“leaky gut”)
- Gut dysfunction fed back into anxiety, low mood, irritability
- This reinforced cravings for ultra-processed foods
A vicious cycle, which eventually ended in the eruption of my small bowel.
Poor gut health is linked with metabolic dysfunction, fatty liver disease, central fat accumulation, and hormonal disruption. Over time, the body becomes less responsive and more reactive.
By contrast, a diverse, well-supported microbiome:
- Reduces inflammation
- Improves stress resilience
- Supports mood, cognition, and immunity
- Enhances physical performance
This is why gut health is not just about digestion — it’s about how you think, move, recover, and show up in life.
Understanding Myself Better
In later years, being diagnosed with high-functioning autism has also given me clarity. With the right professional support, I learned healthier ways to navigate stress, energy demands, and social situations, rather than constantly pushing through them.
The journey I have been talking about in this article took over a decade. I was fortunate to have had medical knowledge, plus able to question the easiest option of recovery - taking medication - and instead of following my internal cues. I was within a clinical setting where my own knowledge and understanding were invaluable to the path I took. Most people don’t have that industry insight or that immediate network of individuals who can help you understand why you are questioning the path of recovery that you are being offered. Most individuals need external support to make the changes that they need for their unique situation, in a safe and sustainable way.
That’s exactly why we do what we do at Uniquely Created U.
Practical Takeaways: Mind-Body-Move®
Mind - Start the day with gratitude. Before checking emails or worrying about problems, speak out or write down three things you’re genuinely grateful for and why. This helps re-focus the mind and reduce stress-driven gut symptoms.
Body - Don’t chase every supplement trend. While vitamin D and creatine have their place, many individuals are chronically low in omega-3 fatty acids, which are essential for gut lining integrity, inflammation control, and brain health. These can come from oily fish or high-quality supplementation.
Move – think about how mobile you are now, and how mobile you would like to be in the future and build a healthy and sustainable habit.
- Sedentary? Start with 15 minutes of walking daily.
- Moderately active? Ensure you mix strength, mobility, and cardio.
- Highly active? Prioritise recovery and fuelling — overtraining without adequate nutrition can damage gut health just as much as inactivity.
Final Thought
Your gut may be influencing your energy, mood, strength, and resilience far more than you realise.
Access our complimentary 4-day food analysis and discover what your gut is really telling you. Discover more here.
