
Vanessa Peat
30 July 2025
Menopause doesn’t just affect your hormones. It ripples through your physical health, mental clarity, relationships, self-identity, and even your ability to connect with those around you. At Uniquely Created U, we hear from women who say they feel like they’re “not themselves anymore.” Not just tired or off-balance but truly lost in a fog of symptoms that are difficult to name, let alone explain.
We believe menopause deserves more than a one-size-fits-all medical response. It requires a compassionate, multidimensional approach that speaks to your emotional, physical, relational, and mental wellbeing.
This blog takes you beyond hot flushes and HRT to explore our mind-body-move® approach to menopause. It’s a compassionate, whole-person perspective that not only supports the woman experiencing menopause, but also the family, partner, or support network walking the journey alongside her.
Our mind-body-move® philosophy matters
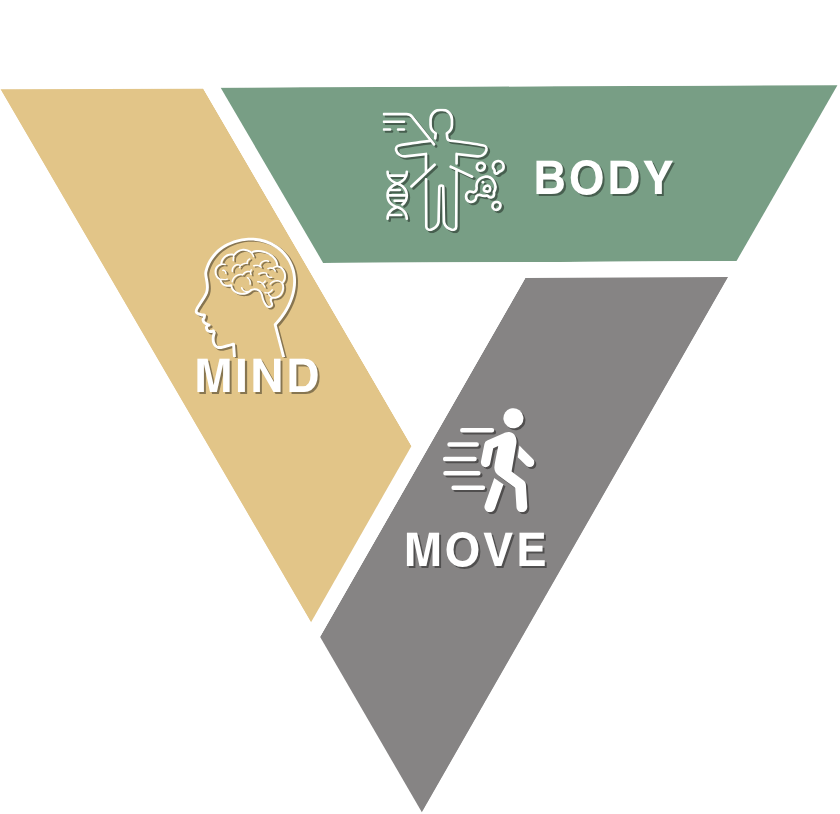
At Uniquely Created U (UCU), we don’t see menopause as a “problem” to fix. We see it as a transition that deserves support, education, and agency. Our mind-body-move® philosophy bridges psychological insight, nutrition science, movement physiology, and relational wellbeing, providing practical tools for real-life change.
Why does this matter? Because menopause is not an isolated event. It intersects with:
- Emotional regulation and mental health
- Energy and motivation
- Intimacy, confidence, and communication in relationships
- Food habits, body image, and metabolism
- Social expectations and the pressure to carry on "as normal"
The invisible symptoms: Brain fog, low motivation & anxiety
Forgetfulness. Mood swings. Lack of focus.
These are often dismissed as “just stress” or “a bad phase,” but for many midlife women, these symptoms mark the onset of perimenopause.
Changes in oestrogen, progesterone, and testosterone impact brain function. UK research confirms that during menopause:
- Cognitive performance is often reduced, especially in memory and verbal fluency
- Mood disturbances, such as anxiety and irritability, are more likely to surface
- Low motivation and reduced coping ability are common⁽¹⁾
This isn’t a mindset ‘problem’, it’s a neurological and hormonal shift. That’s why lifestyle strategies that include emotional expression, nourishment, rest, and movement are essential.
Relationships under pressure: The unspoken impact

Menopause doesn’t just affect the woman going through it. It impacts everyone close to her, especially partners and family.
Many women report increased tension at home, decreased libido, misunderstandings around mood, or feeling emotionally disconnected. And many partners simply don’t know what’s happening or how to help.
The UK charity Menopause Matters and the British Menopause Society have both emphasised that family and partner support is a protective factor for mental health during menopause.⁽²⁾ Lack of understanding, however, can increase stress, shame, and isolation.
That’s why at UCU, we encourage conversations that bring partners into the picture. We help families understand:
- That menopause is not about “moodiness”, it’s a real biological transition
- That compassion and communication are more helpful than fixing or minimisingThat joint support strategies (like shared exercise, meals, or mindfulness) can strengthen relationships, especially during this period
A cultural shift is needed

Despite increased awareness, menopause is still misunderstood and often trivialised. Women are told they’re “just getting older” or advised to “power through,” creating a stigma that silences real suffering.
In many workplaces and communities, there's still a lack of meaningful menopause support. According to a 2022 UK Government report, nearly 1 in 10 women leave their jobs due to menopause symptoms ⁽³⁾.
The toll is not just physical, it’s emotional, economic, and social. But it doesn’t have to be this way.
At UCU, we believe in reclaiming this life stage as a time of rebalancing, not breakdown. With the right tools, support, and understanding, menopause can become a turning point, a catalyst for clarity, strength, and new purpose.
The role of boundaries and self-care
Many women reach midlife while still carrying the invisible load of caregiving, emotional labour, and work stress. When menopause symptoms appear, the ability to cope often collapses under the weight of unspoken responsibilities.
That’s why we integrate emotional boundaries and self-leadership into our menopause care.
Boundaries are not selfish, they are the oxygen mask women often need to put on first. We support our clients to:
- Say no to overcommitment without guilt
- Set new rhythms of rest, reflection, and reconnection
- Recognise burnout triggers and step back with grace
- Ask for, and accept, help
This kind of self-care goes far beyond the realm of considering a spa day. It’s about reclaiming time, space, and worth in a season where everything feels in flux

Lifestyle Medicine: What makes the UCU approach different?
At UCU, we use a whole-person, evidence-informed approach that addresses the root causes of menopause-related challenges, while recognising that menopause affects every system of your body and every area of your life.
Here’s what’s included in our mind-body-move® Menopause Support Pathway.
1. Mindfulness and cognitive rebalancing
We introduce evidence-backed practices such as breathwork, meditation, gratitude journaling, and CBT-informed strategies to manage anxiety, brain fog, and emotional overwhelm.
2. Relational wellbeing
We offer guidance on navigating changing intimacy, communication, and connection, as well as partner and family education tools to improve understanding and empathy. We understand that support needs to be tailored differently for solo parents, carers, or women navigating menopause alone.
3. Boundaries and self-leadership
Our coaching helps you to redefine roles and responsibilities in work and family life and supports you in setting healthy boundaries without guilt. Reframing self-care can be extremely difficult but needs to be readdressed and realigned to meet your changing physiology while still meeting your daily functional needs.
4. Nutrition for hormonal balance
We help you understand what your body needs now, from blood sugar regulation to gut-brain support to inflammation reduction. We include anti-inflammatory foods, phytoestrogens, and tailored plans for symptoms like weight gain or increased fatigue. Our nutrition strategies not only address hormonal balance but bone health and energy restoration, while addressing any additional support for sensory, behavioural, and digestive differences experienced by neurodivergent individuals, or those with gut health issues such as IBS or IBD.
5. Movement that supports you
Rather than ‘just pushing harder’ to try and improve your overall visual physical appearance, we guide you toward tailored functional movement that energises your nervous system and supports bone, brain, and metabolic health. Think low-impact resistance training, Pilates, walking, or restorative yoga.
6. Personalised support and optional referrals
Whether you need HRT support, counselling, or more in-depth assessments, our in-house team, including a GP, dietitian, nutritionist and behavioural change specialist, ensures your plan is truly integrative.
What partners and families need to know
Menopause is a team sport.
We encourage partners and family members to:
- Ask rather than assume: “How can I support you today?” is more powerful than advice.
- Learn about symptoms and triggers: Understand how symptoms may vary and why they’re not simply “mood swings.”
- Be present, not perfect: You don’t need all the answers. Your presence can be just as powerful.
- Create space for joy and connection: Laughter, shared rituals, and intimacy may change, but they don’t have to disappear.
When support networks show up with curiosity and compassion, they can become anchors during this season of change.
Menopause as a new beginning — not the end
Menopause is often framed as the end of something, fertility, energy, or femininity. But at Uniquely Created U, we see it as a powerful rebalancing, a shift toward a new rhythm that allows women to live more freely, confidently, and in alignment with who they now truly are.
Our Mind-Body-Move® Menopause Support Programme is designed to:
- Provide tailored, expert-backed strategies for whole-life wellbeing
- Offer professional guidance without judgement
- Restore clarity, energy, and confidence at your pace
It’s a time to re-evaluate, re-energise, and reconnect to your body, your needs, your relationships, and your future.
Ready to take the next step in your journey?
We’re opening spaces for our next Mind-Body-Move® Menopause Support Pathway, for women who want to feel their best every day.
A transformative 8-week journey designed for women who want to protect their future health, regain vitality, and make confident, evidence-based choices. Each week, you’ll unlock practical, expert-led guidance grounded in clinical insight and nutritional science.
This Masterclass is grounded in our Mind-Body-Move® philosophy, designed to move you out of survival mode and into sustainable strength and wellbeing.
8-Week Women’s Health Masterclass next start date: January 2026.
We currently have an Early Bird Exclusive Option: £224
(Saving 20%) available until 30 September 2025
Click here to find out more and secure your spot today.
Future-proof your health with clarity and confidence.
References
- Public Health England. (2017). Health Matters: Obesity and the Food Environment. https://www.gov.uk/government/publications/health-matters-obesity-and-the-food-environment
- Jackson, S. E., Kirschbaum, C., & Steptoe, A. (2017). Hair cortisol and adiposity in a population-based sample of 2,527 men and women aged 54 to 87 years. Obesity, 25(3), 539–544. https://pubmed.ncbi.nlm.nih.gov/28229550/
- NICE. (2015). Menopause: diagnosis and management (NG23). https://www.nice.org.uk/guidance/ng23
- NICE. (2023). Semaglutide for managing overweight and obesity (TA875). https://www.nice.org.uk/guidance/ta875
- Fowler, N., Griffiths, C. A., & Baird, A. (2022). Between- and within-person effects of stress on emotional eating in women: a longitudinal study over 49 days. Psychological Medicine, 53(11), 5167–5176. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10471857/
- Larsen, J. K., van Strien, T., Eisinga, R., & Engels, R. C. M. E. (2017). Depressive symptoms and weight in midlife women: The role of stress eating and menopausal status. Midlife Women’s Health, 3, 6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5607068/
